Advancing Responsible Opioid Prescribing
Supporting Ambulatory Providers Through Clinical Education, Training, and Technical Assistance
Research Brief | May 24, 2017
Background
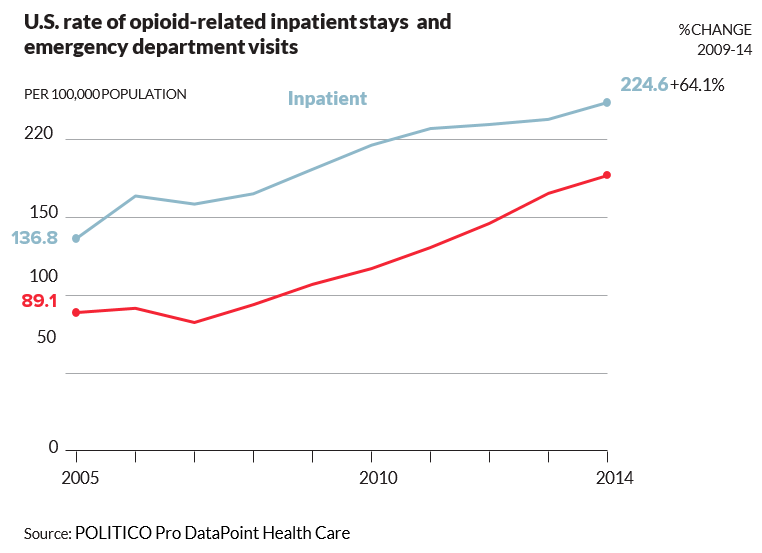
Each day in the United States (U.S.), more than 50 people die from an overdose of prescribed opioid pain medication, and over 1,000 people are treated in an emergency department (ED) for misusing prescribed opioids.1 According to the Centers for Disease Control and Prevention (CDC), opioid overdose deaths now eclipse traffic accidents as the leading cause of death in adults aged 25–64.2 The majority of these deaths are attributable to a legitimate prescription written by a medical provider.3 In fact, in 2012, there were enough opioid prescriptions in the U.S. for every American to have a month’s supply of opioid pain medication. Accordingly, sales of opioids increased, quadrupling from 1999 to 2014.1 Yet despite this increase, there has been no change in the amount of pain Americans are reporting.4 A recent CDC study suggests that even a 10 day supply of opioids is associated with a significant increase in the likelihood of long term opioid use.5
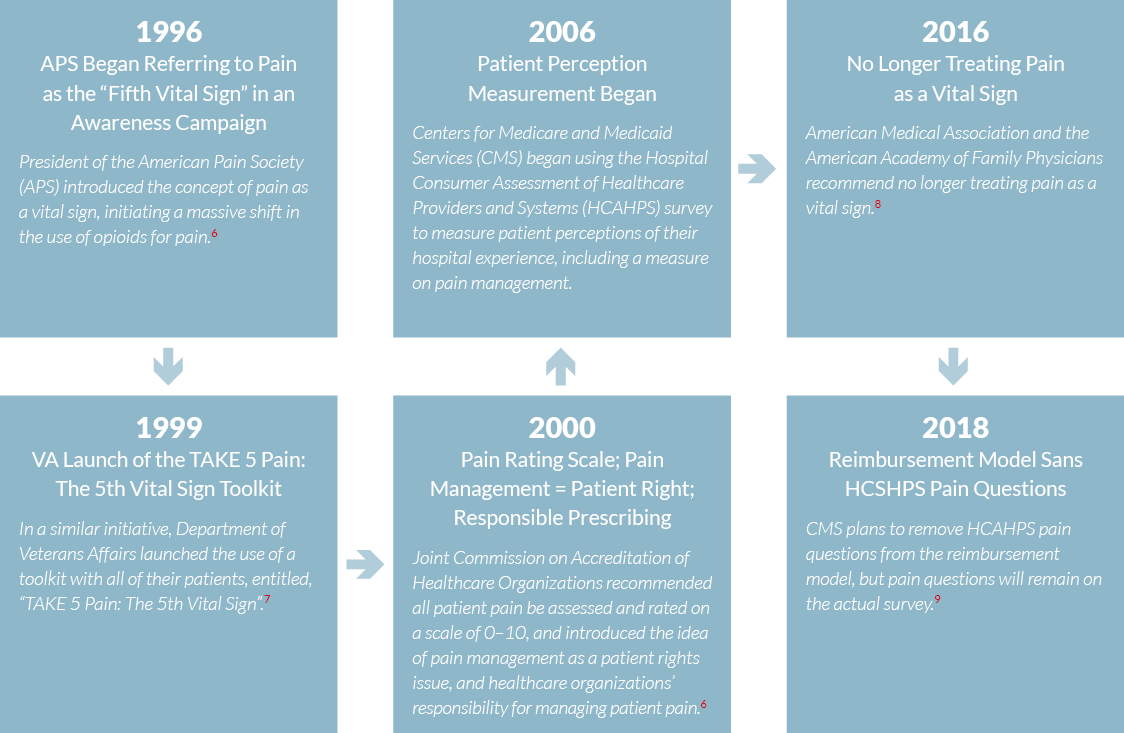
Spanning over two decades, the following are key events related to the current opioid epidemic:
A Need for Effective and Efficient Solutions
Today, many providers struggle with patient pain management, and are not prepared to initiate safe pain management therapies. This includes opioid prescribing, even when warranted. Providers lack education, training, and tools to perform appropriate risk assessment, prescribing, and monitoring to prevent opioid dependency or misuse. This raises the concern that many patients may find it harder to find someone willing to appropriately address and manage their pain.
In April of 2017, the Department of Health and Human Services (HHS) announced $485 million dollars in grants to help states combat opioid addiction. While the majority of the award in the first year is intended to address urgent treatment and recovery activities, in subsequent years, HHS will continue to provide funding to support policies that are “the most clinically sound, effective and efficient”, including five prioritized strategies: strengthening public health surveillance, advancing the practice of pain management, improving access to treatment and recovery services, targeting availability and distribution of overdose-reversing drugs, and supporting cutting-edge research.10
How We Can Help
Altarum is at the forefront of efforts to address behavioral health issues in the U.S., especially those related to addiction, treatment and recovery, opioid use and abuse, continuing integration of mental health and addiction service systems, and the concurrent integration of behavioral health with physical health systems under the Patient Protection and Affordable Care Act (ACA). Altarum’s work within the healthcare system includes behavioral health policy analysis, health services research, evaluation, technical assistance (TA), medical education, and training.
Altarum’s Behavioral Health Coordinating Center works to promote empowerment and choice, foster resilience, and facilitate mental health and addiction recovery for individuals, families, and communities. Altarum works with federal, state, and local governments, national and local organizations, and providers that are on the frontlines of addressing critical behavioral health issues from prevention to recovery. Our work actively involves individuals and their families to create a patient-centric care approach that drives local practice-level solutions to meet complex care needs. Altarum also works with community boards, managed care organizations, community mental health centers, and state directors to address changes in behavioral health policy. These relationships provide Altarum with a unique understanding of essential health benefits, how they affect behavioral health services, and the importance of having clients and their families involved in shared decision making.
In addition, Altarum has developed a unique joint providership with the University of Michigan Medical School and Health System to offer robust medical education and training programs that address chronic and emerging gaps in care through upstream prevention based approaches. Specifically, our programs tackle a number of critical issues related to chronic disease, behavioral health, and medication management facing health care providers today (i.e. Responsible Opioid Prescribing, Depression Screening, Medication Adherence, and Pediatric Oral Health in Primary Care). Performance Improvement CME and Maintenance of Certification (MOC) Part IV credits are offered as part of these quality improvement training programs to drive behavior change. These credits allow physicians, nurse practitioners, and physician assistants to meet their state licensure and board certification requirements. This affiliation also allows Altarum to provide MOC Part IV credits to providers certified through the American Board of Medical Specialties (ABMS) member boards.
Advancing Responsible Opioid Prescribing
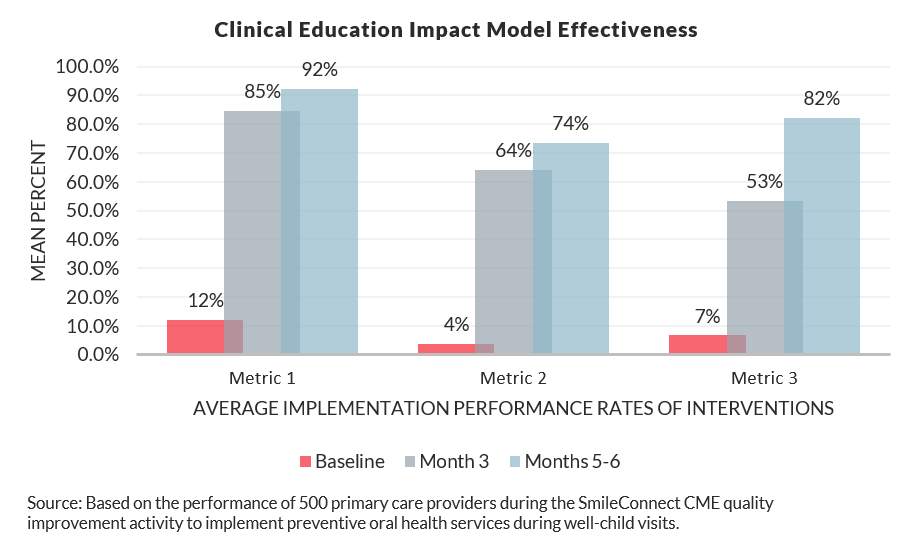
Altarum provides training and support tools through our Advancing Responsible Opioid Prescribing program to improve conscientious prescribing, patient education, and prescription tracking (utilizing Prescription Drug Monitoring Programs) among ambulatory providers. This program compliments the current focus on treatment and recovery by offering states, health systems, and other stakeholders an opportunity to reduce the impact of the opioid epidemic through prevention. Eligible participants earn 30– 50 CME and 20–25 MOC Part IV credits for attending a one hour training, aligning clinical care processes to support quality improvements, and monitoring and measuring their performance for six months by conducting patient chart reviews. Through the combination of CME and MOC Part IV credit, on-demand technical assistance, and rigorous quality monitoring, Altarum has achieved impressive results in physician behavior change from pre-training baseline to six months post-training. Topic area aside, Altarum’s clinical education impact model provides dramatic and sustainable results related to clinical-based interventions.
The Advancing Responsible Opioid Prescribing program strengthens workforce capacity to address unsafe opioid prescribing and mitigate the impact of the opioid epidemic on children, families, and seniors. We are poised to begin training over 5,000 providers and improving care for ~1M patients across the Midwest. We anticipate at least a 50% increase in the number of patients evaluated for risk of opioid misuse, and a 50% increase of patients with documented follow-up evaluations. Prescription Drug Monitoring Program (PDMP) registration is a required component of our TA, and significant increases in PDMP use is expected. Our program is fully scalable, and we have the infrastructure in place to expand this critical work beyond the Midwest to other states that have prioritized prevention strategies.
Sources
- Rudd, R.A., Seth, P., David, F., & Scholl, L. (2016). Increases in Drug and Opioid-Involved Overdose Deaths – United States, 2010-2015). MMWR, 65(50-51), 1445-1452.
- Centers for Disease Control and Prevention. (2011). Vital Signs: Overdoses of Prescription Opioid Pain Relievers – United States, 1999-2008. MMWR, 60(43), 1487-1492.
- Jones, C.M., Paulozzi, L.J., & Mack, K.A. (2014). Sources of Prescription Opioid Pain Relievers by Frequency of Past-Year Nonmedical Use. JAMA Internal Medicine, 174(5), 802-803.
- Chang, H., Daubresse, M., Kruszewski, S., Alexander, G.C. (2014). Prevalence and treatment of pain in emergency departments in the United States, 2000 – 2010. American Journal of Emergency Medicine, 32(5), 421-31.
- Centers for Disease Control and Prevention. (2017). Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use—United States, 2006-2015. MMWR, 66(10), 265-269.
- Phillips, D.M. (2000). JCAHO Pain Management Standards are Unveiled. JAMA, 284(4), 428-429.
- The Department of Veterans Affairs. (1999). Take 5 Pain: The 5th Vital Sign. The Department of Veterans Affairs.
- Lowes, R. (2016). Drop Pain as the Fifth Vital Sign, AAFP Says. Medscape, September 22, 2016.
- Hospital Consumer Assessment of Healthcare Providers and Systems. (2016). CMS Finalizing Removal of the Pain Management Dimension from Hospital Value-Based Purchasing in FY 2018.
- U.S. Department of Health and Human Services. (2017). Trump Administration awards grants to states to combat opioid crisis. Press release.
